Vulnerable Britain: Can Tech Help Social Care?
Britain’s health and social care systems are ailing. Strapped for cash, its public services are straining to meet unprecedented demand from an ageing population. The number of people aged 85 and older needing 24-hour care is on course to double, according to a recent report by Newcastle University’s Institute for Ageing, which warns that the social care system is “at breaking point.”
Published in The Lancet in August 2018, the report comes ahead of Government plans to reform adult social care and the National Health Service (NHS) and states that the number of 65-year-olds and over needing round-the-clock assistance is also set to rise by a third. Many such “high dependency” adults will develop multiple long-term health conditions, such as obesity and diabetes, creating increasingly complex care needs.
Not what the doctor ordered
These are uncertain times for the NHS as Britain prepares to leave the EU next year. Brexit is likely to deal blows to its workforce and finances. The healthcare sector relies heavily on migrant EU staff, yet last year record numbers of frontline medical staff quit Britain. By 2030, some 90% of the UK’s population will be city dwellers and more of the elderly will live with dementia and in isolation. Faced with declining State support, councils will have to embrace new ways to attract investment and create wealth. At present, public services are compartmentalised and sometimes incompatible; the remedy is to shatter bureaucratic silos, and limit procurement and compliance red tape.
Disrupting the public sector
Smart cities can work if local authorities pool know-how, resources and costs for “interoperability” across all services, for example, local and central governments; health services and utilities; and smart tech providers. Technology can help streamline procedures and address old problems efficiently, for example, Blockchain could enable secure, easy transactions between governments, councils, boroughs and authorities, while also fostering digital business integrity. Mobile devices, too, can help the care network make the shift to paperless communication.
The Smart Citizen looks at three UK cities and regions taking on 21st century challenges by overhauling outmoded systems, making them fit for purpose and, importantly, keeping users’ concerns uppermost.
Bristol: Connecting Care, coordinated services
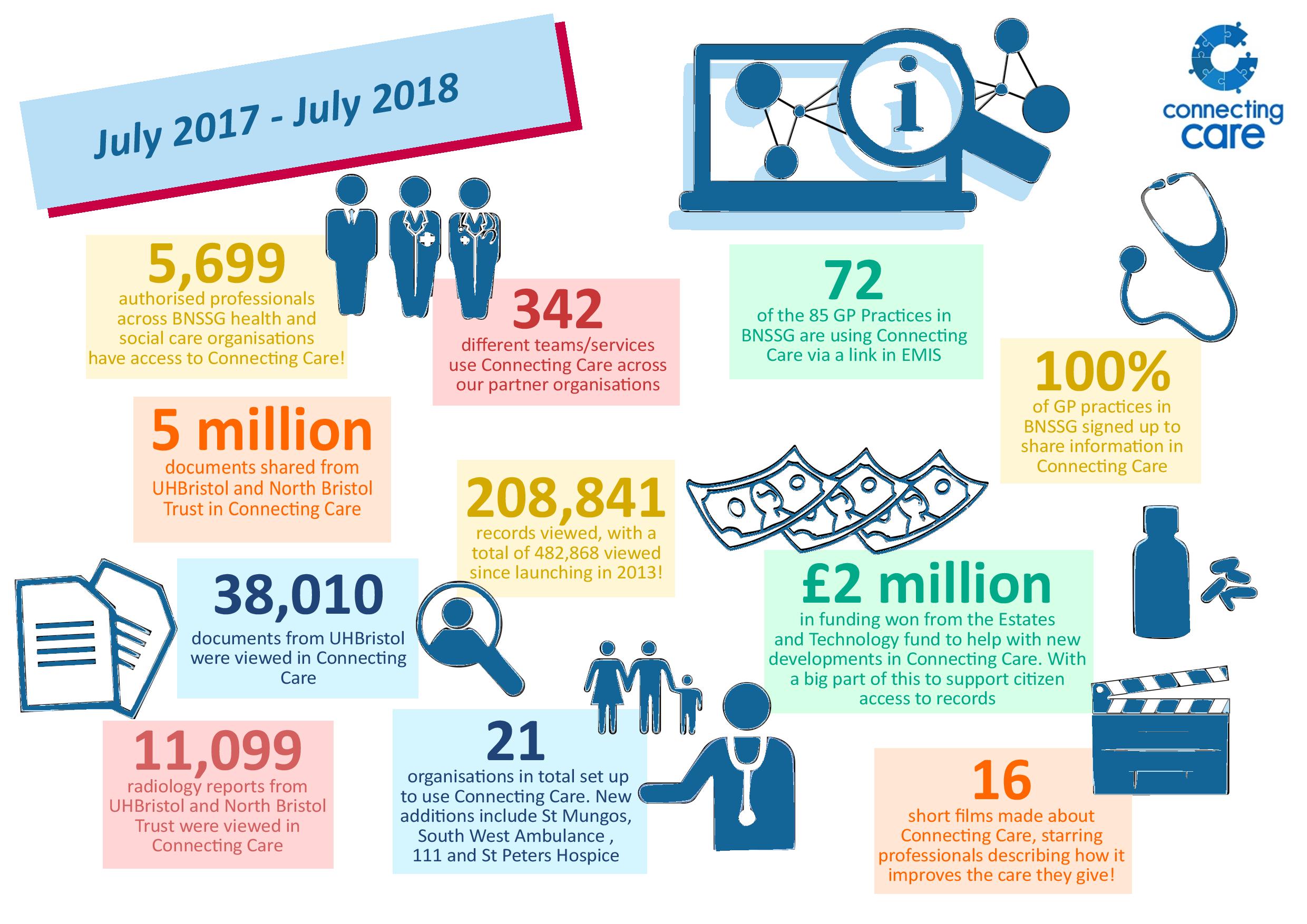
To most people the NHS is a vast umbrella; in reality it is a fragmented service whose networks don’t talk to each other. Take Bristol, where 17 health and social care organisations deal with nearly one million people in Bristol, North Somerset and South Gloucestershire. Until recently, getting an NHS trust to share data with a local authority was a challenge as each body adheres to its own governance structures. The Connecting Care partnership links up three trusts, two mental health trusts, GP and out-of-hours practices, ambulance services, local authorities and community healthcare providers, among others. Andy Kinnear, Director of Digital Transformation, South, Central and West Commissioning Support, explains: “Connecting Care began life in 2011 when a group of digital leaders got together to see if they could begin joining electronic patient records together to create a single view of the combined record.”
Kinnear advocates breaking down the boundaries between health and social care organisations. “The driver was a burning desire to ensure our clinicians and care professionals had the information about our patients in front of them at the point of care. Today over 5,000 professionals are accessing 200,000 combined records every year making safer, faster and better decisions.”
Coordinated healthcare is critical to the safe functioning of the NHS but its practitioners are sometimes negotiating an unconnected network. For example, GPs retain patients’ histories, while hospitals and mental health practitioners possess details on specific treatment. And time that could be spent saving lives, for example, in a busy Accidents & Emergency department of a hospital, is wasted trying to make sense of confusing information on random bits of paper or phoning around to check a patient’s prescription or allergies.
Connecting Care is an integrated digital portal that ensures interoperability between disparate systems and real-time information-sharing. Everyone sees the same data. Staff can quickly look up patient demographics, laboratory results, radiology, diagnoses, medications, problems and procedures. Importantly, patients are spared the stress of remembering and repeating their medical history ad nauseam. About 50% of people who use Bristol’s social care services are aged 75. The portal represents a win-win for community healthcare, allowing more early interventions to take place. Social workers see who else is involved in a patient’s care and log their assessments. “In cases where we are dealing with a person who is being supported by Rapid Response and the district nurses, Connecting Care comes in to its own. All the notes from visits are documented and it can save at least 30-40 minutes on duty cases of this nature,” according to one social worker.
“Creaky systems cost lives,” said UK health secretary, Matt Hancock, who has just pledged £200m to upgrade technology. Building a tech-savvy NHS may not seem pressing; yet, he believes a reactive service driven more by internal targets and outcomes than by users’ needs is “downright dangerous.” So, Kinnear is rightly proud of what Connecting Care has achieved.
Cornwall: E-health and e-wellbeing
Pockets of intense deprivation characterise Cornwall’s largest urban area, made up of the former tin mining towns of Camborne, Pool, Illogan and Redruth. Cornwall has received more EU funding than anywhere else in Britain in the past 20 years. European subsidies have paid for massive investments in local infrastructure and, indeed, enticed new technology-based industries. Yet, Cornwall registered a higher proportion of ‘leave’ voters in the Brexit referendum than the UK average.
“Cornwall faces a number of challenges. It has an ageing population, with high demand for health and social care,” says Dr. Tim Taylor, Senior Lecturer in Environmental and Public Health Economics, who is Principal Investigator of Smartline, a digitally connected community backed by a group of epidemiologists, economists, geographers, mathematicians and sociologists.
As part of Smartline, social landlord Coastline Housing is working to fit 350 homes with environmental sensors to monitor indoor air pollution, energy and water consumption, temperature and heating efficiency. Researchers use the data to promote the community’s resilience to such issues as cold, damp, mould and fuel poverty. They can get an idea of what is driving health issues, for example, if residents are sedentary, if areas have a high incidence of asthma or if people are living in social isolation. Cornish businesses will also benefit: the data are being made available to help develop new apps and technologies.
Smartline is led by the University of Exeter in partnership with Coastline Housing, Cornwall Council and Volunteer Cornwall. Its total budget £4.75 million is funded by the European Regional Development Fund (ERDF) and the South West Academic Health Science Network. How will it raise support once EU regional funding dries up? Dr. Taylor explains: “Brexit is a source of considerable uncertainty in terms of removing access to European funding for the regions. The political parties in the UK seem committed to providing funds to replace those lost, but it is yet to be seen quite what form the funding will take and how much will be provided”. Much is at stake: “Cornwall has gained a lot from European funds and I hope Smartline will have a legacy beyond the ERDF funding for Cornwall to be able to build on in developing e-health and e-wellbeing solutions,” said Taylor.
Bradford: IoT addresses elderly isolation and assisted living
Yunus Mayat describes Bradford as a “risk-taking city.” The Enterprise Architect and Information Manager from Bradford Council wants Internet of Things (IoT) devices to help improve health in a region where 1 in 10 people over 50 are not receiving care. From a pilot project using 10 tablets, 100 have now been made available at no cost to the user. Central to these efforts is the deployment of LoRaWAN (Low Range Wide Area Network) and narrow band IoT for low-power wireless connectivity.
Bradford District’s population of over-65s will number 108,000 by 2035, 40% more than 2010. To promote independent living, Bradford has trialled room and pressure sensors that monitor lights, curtains and doors, while other devices read heartbeat and blood pressure and check for falls. Unusual behaviour patterns can be detected, thus alerting health or social workers to problems, such as wandering.
The city has pioneered the use of secure 4G internet-based homecare tablets developed by tech start-up Konnektis, which aims to provide homecare workers, family members and medics with a complete picture of a senior patient’s needs and help manage all aspects effectively – from nutrition, medication, hydration to sleep. Digitally stored data are presented live, so homecare staff can spot any missed support or clinical interventions and act swiftly. Relatives can check when their loved one was last visited or contact carers.
A looming funding gap of £5.8 billion by 2019/20 threatens to erode adult social care even further. Mayat says he is concerned, but local governments need to demonstrate that living at home longer reduces the expenses of hospital beds and care homes. “If we can provide a business case to show value and savings, this would help bring much-needed funding to make things happen. This was true about Konnecktis – starting small and scaling up.” Procurement must also be simplified; the SME developed the platform and tablet application to eliminate the need for lengthy tenders, explains Mayat, and service providers can also be billed more cost-effectively for their time.
Doing more with less
The NHS is dogged by financial woes. Councils are struggling without a sustainable funding strategy to underpin social care. The onus is on public services to safeguard high-quality care, ditch entrenched practices and apply tailor-made technological solutions. Digital integration cannot cure all the ills besetting the NHS but it does represent a valuable investment.
The prognosis need not be bleak; opportunities, too, are arising to create a society that supports its most vulnerable and improves their quality of life.
Interviews with city stakeholders were facilitated by media partner Informa at Smart to Future Cities, the next edition of which will be held from 10 to 12 April, 2019 at ILEC Conference Centre, London.
Featured Image: Coastline Social Housing, Cornwall

